

Of the women included in the national registry, 78% had ruptured membranes. All of the cases noted during caesarean section had their onset soon after delivery of the infant.Ī factor that is consistently related to the occurrence of AFE is a tear in the fetal membranes. In the national registry, 70% of the cases occurred during labor, 19% were recorded during caesarean delivery, and 11% occurred after vaginal delivery. The syndrome typically occurs during labor, soon after vaginal or caesarean delivery, or during second-trimester dilation and evacuation procedures. The incidence of AFE has been reported to range from 1 in 8000 to 1 in 80,000 deliveries. Clarke et al., in the United States, and Tuffnell in the United Kingdom have established a national registry for suspected AFE.Įntry criteria consist of the presence of the following four factors: Because AFE is so uncommon, no single institution has sufficient experience to assess risk factors, determine the pathophysiology and clinical course, or evaluate management strategies. Clarke et al., have proposed renaming the syndrome “anaphylactoid syndrome of pregnancy” because of the various humoral and immunologic factors implicated. These findings formed the “classic” pathologic findings in AFE.Īlthough historically the pathophysiology was thought to involve embolization of amniotic fluid, there has been growing evidence that the syndrome results from bronchial mediators that are released after embolization occurs. The histopathology of the pulmonary vasculature of these women included mucin, amorphous eosinophilic material, and squamous cells. The importance of this condition and these early studies was not established until 1941, when Steiner and Lushbaugh reported the clinical and pathological findings of 42 women who died suddenly during or just after labor. It was reported again in an experiment on laboratory animals by Warden in 1927. We have searched PubMed using keywords like amniotic fluid, amniotic fluid embolism, embolism, catastrophe, disseminated intravascular coagulation, hypoxia, and pregnancy either alone or in combination for reviewing this topic.Īmniotic fluid embolism was first reported by Ricardo Meyer in 1926. Furthermore, despite advances in the care of critically ill patients, no management interventions have been found to improve the survival or long-term outcome of woman with AFE. Understanding its etiology and pathophysiology is incomplete, and the criteria used to make its diagnosis are controversial. In some women AFE may lead to mild degree of organ dysfunction while in others it may lead to coagulopathy, cardiovascular collapse, and death. In addition, elements of amniotic fluid have been isolated in blood and sputum of pregnant women who did not have clinical evidence of AFE. AFE is initiated by entry of amniotic fluid into the maternal circulation and is characterized by the sudden onset of severe dyspnea, tachypnea, and cyanosis during labor, delivery or early puerperium, the mechanism of which is unclear. Given its sudden and dramatic presentation and its often devastating consequences, practitioners given the responsibility of caring for an unfortunate woman with AFE remember the experience in great detail for a long time thereafter.
Despite improved modalities for diagnosing AFE, and better intensive care support facilities, the mortality is still high.ĭespite its rare occurrence, the syndrome of amniotic fluid embolism (AFE) is well-known to anesthesiologists.
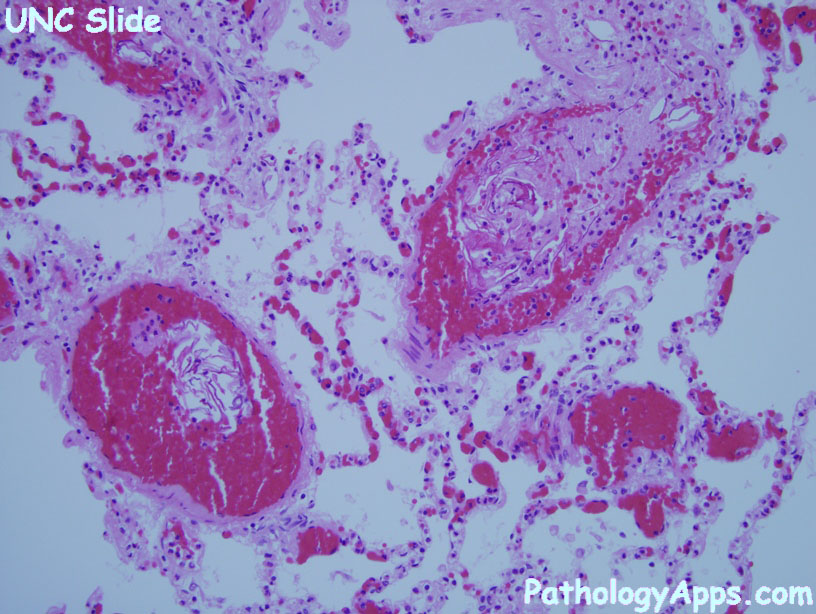
The cornerstone of management is a multidisciplinary approach with supportive treatment of failing organs systems. Usually the diagnosis is made clinically and by exclusion of other causes. Definite diagnosis can be confirmed by identification of lanugo, fetal hair and fetal squamous cells (squames) in blood aspirated from the right ventricle. Undetected and untreated it culminates into fulminant pulmonary edema, intractable convulsions, disseminated intravascular coagulation (DIC), malignant arrhythmias and cardiac arrest. The pathophysiology is believed to be immune mediated which affects the respiratory, cardiovascular, neurological and hematological systems. AFE can occur during labor, caesarean section, dilatation and evacuation or in the immediate postpartum period. Unfortunately, this situation has very grave maternal and fetal consequences. The underlying mechanism for AFE is still poorly understood. The disastrous entry of amniotic fluid into the maternal circulation leads to dramatic sequelae of clinical events, characteristically referred to as Amniotic fluid embolism (AFE).


 0 kommentar(er)
0 kommentar(er)
